Rugpijn & nekpijn
Hernia (nek of rug)
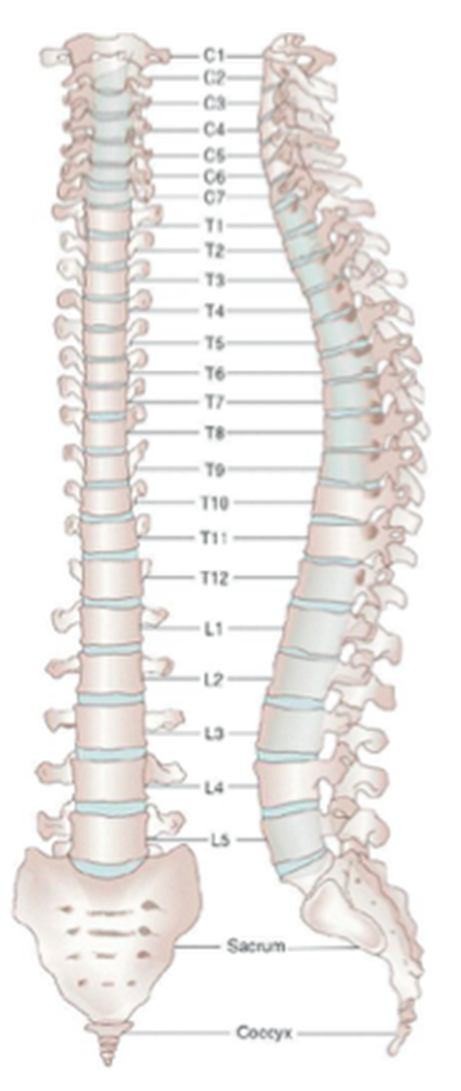
Hernia is een van de meest voorkomende wervelzuilaandoeningen. Er bestaan rughernia's (= lumbale discushernia) en nekhernia's (= cervicale hernia).
Wat is een hernia?
Vooraleer we ingaan op de behandelingswijze van deze aandoening, is het goed om even stil te staan bij wat een discushernia (kortweg ‘hernia') precies is.
Tussen onze wervels zit een discusvormige schijf. Die zorgt ervoor dat de wervels onderling niet tegen elkaar stoten en gemakkelijk tegenover elkaar kunnen bewegen. Deze tussenwervelschijf bestaat uit een buitenring van stevig, vezelachtig kraakbeen en bevat een weke, geleiachtige kern. Het is deze kern die zorgt voor de veerkracht en het schokdempend effect van de wervelkolom tijdens het bewegen.
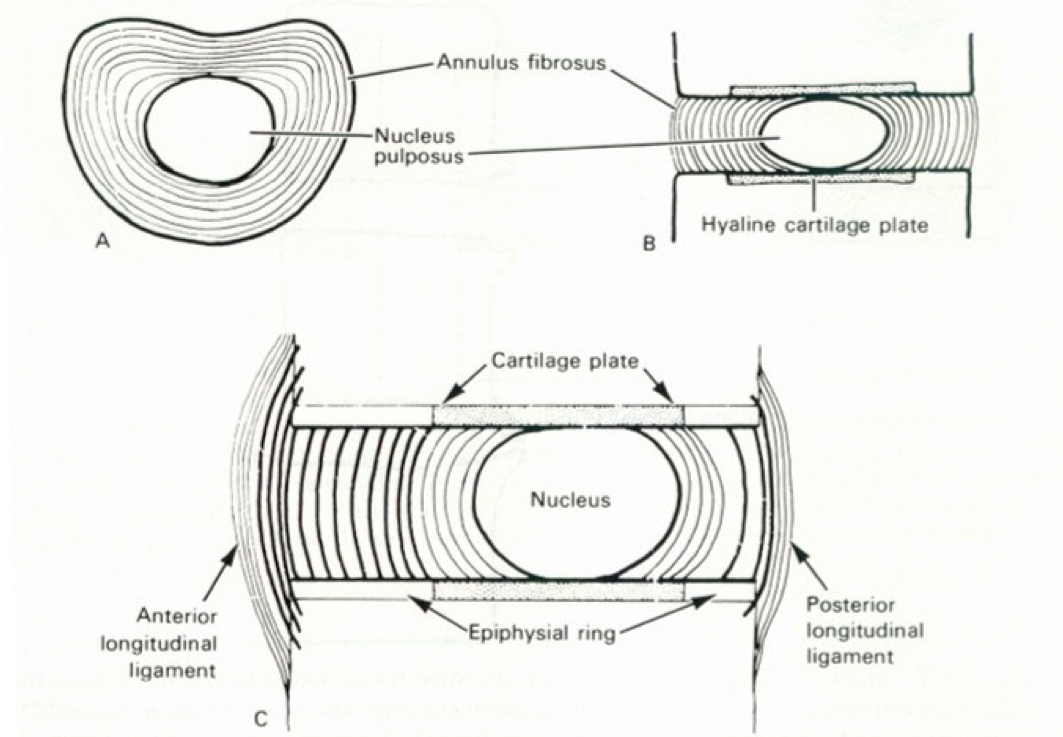
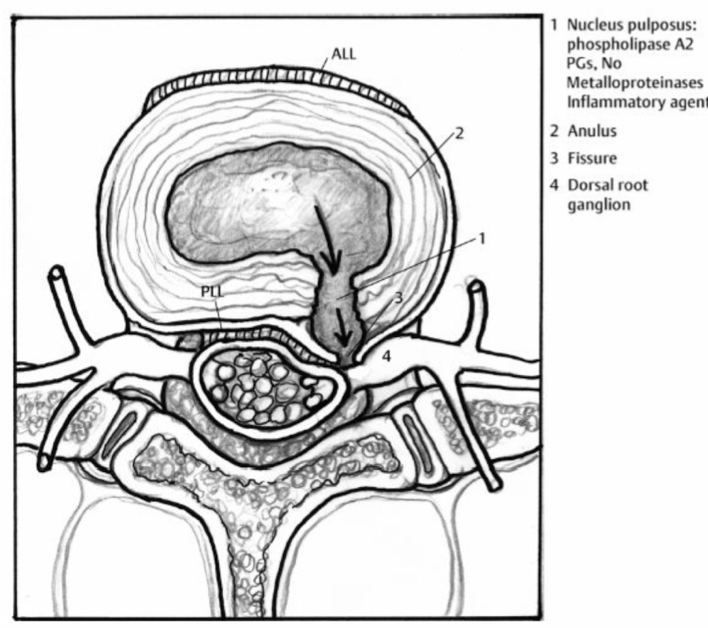
Zodra de buitenring (annulus) van de tussenwervelschijf scheurt (bvb door overbelasting van de rug, een verkeerde beweging of een ongeval), kan de geleiachtige kern uitpuilen en zo de zenuw irriteren of zelfs gedeeltelijk afklemmen. Dit leidt tot uitstralingspijn tot in de benen of armen. In de ergste gevallen kunnen zelfs verlammingsverschijnselen optreden.
De naam hernia komt uit het Latijn en betekent 'breuk'; deze term verwijst naar de uitstulping of scheur van de annulus van de tussenwervelschijf.
Rughernia en nekhernia
De meeste discushernia's komen voor in de onderste drie
segmenten van de wervelkolom (= lumbale discushernia). Maar ook in
de halswervelkolom komt een hernia regelmatig voor (= cervicale discushernia).
De uitstulping van de tussenwervelschijf kan rechtstreeks
op een zenuwwortel drukken en zo een intense pijn veroorzaken. Daarnaast
kan een zenuw die te lang gekneld zit permanent beschadigd worden met als
gevolg blijvende pijn, gevoelsstoornissen en verlamming. Hierdoor is het
vaak aangewezen om de uitstulping operatief te
verwijderen. Zo wordt de zenuwfunctie hersteld en verminderen of verdwijnen
de klachten van de patiënt.
Minimaal invasieve techniek voor minder pijn en vlotter herstel
In het Onze-Lieve-Vrouwziekenhuis wordt standaard een 'discectomie door transmusculaire tubes' (minitubes) gebruikt voor rugoperaties. Daarbij wordt de operatieve microscoop gebruikt of kan een endoscoop gebruikt worden (micro-endoscopische discectomie of MED).
Deze 'kijkoperatie' of 'minimaal invasieve techniek' zorgt ervoor dat het weefsel zo min mogelijk beschadigd wordt. Als patiënt lijdt u minder pijn, hoeft u minder lang in het ziekenhuis te blijven en zult u vlugger genezen.
Rugoperatie vroeger: ingrijpend en pijnlijk
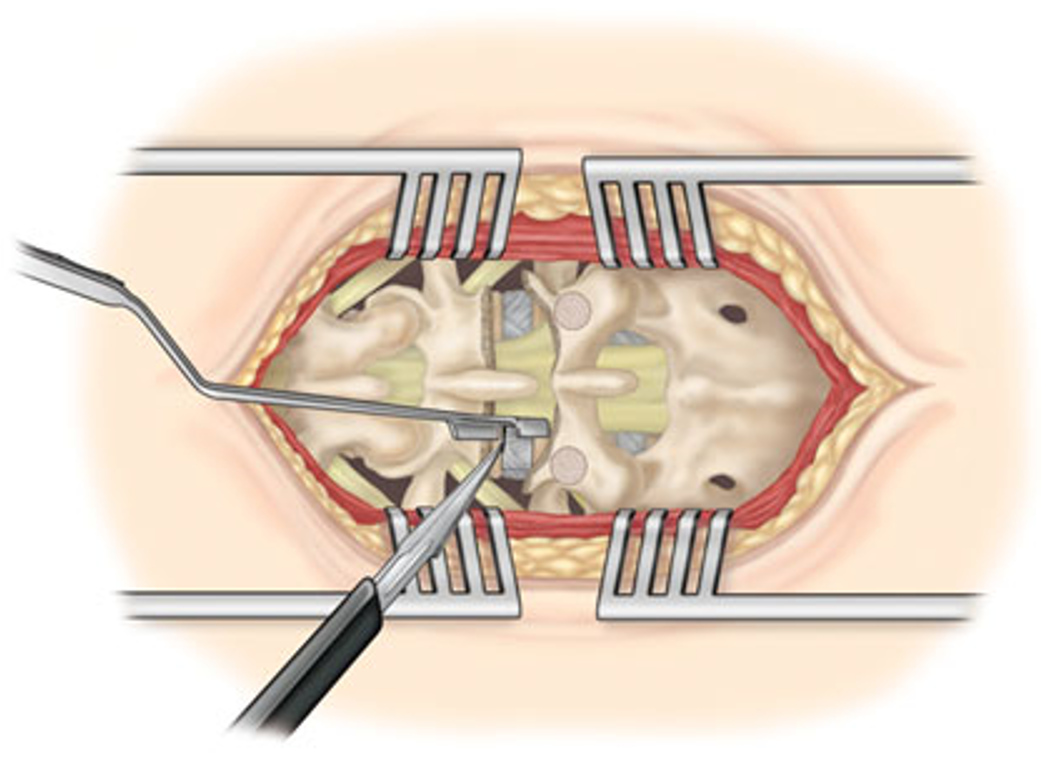
Hierboven de klassieke incisie: de spieren moeten ver uit elkaar gespreid worden en dit geeft aanzienlijke pijnklachten na de operatie.
Rugoperatie vandaag: minimaal invasief voor sneller herstel
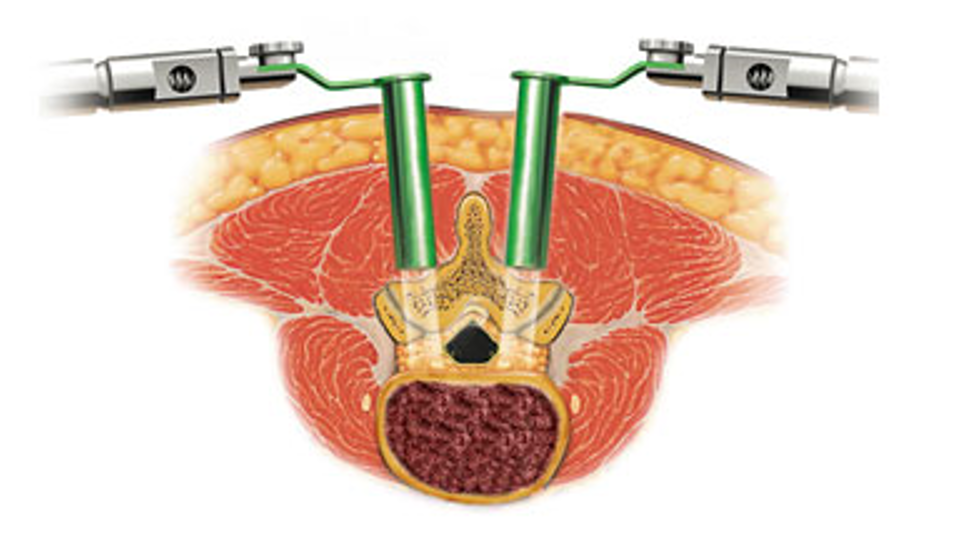
Hoe wordt een lumbale discushernia (rughernia) geopereerd?
Als pijnbehandeling en rust geen verlichting van de klachten brengen, is een operatie vaak het laatste redmiddel. Waar een herniaoperatie vroeger een ingrijpende medische ingreep was, is dat tegenwoordig gelukkig helemaal anders. Hernia's worden behandeld met een transmusculaire tube, geholpen door een microscoop of endoscoop. We spreken hier dan voor microendoscopische discectomie (MED).
De operatie gebeurt aan de hand van kleine kokertjes 'minitubes' die in de rug worden ingebracht, via een zeer kleine incisie door de huid ter hoogte van de tussenwervelschijf waar de hernia zich bevindt.
De uitstulping van de discus wordt met fijne instrumenten via deze kokertjes verwijderd. Hierdoor verlicht onmiddellijk de druk op de zenuw, waardoor de pijn na de operatie meestal ook direct vermindert of zelfs helemaal verdwijnt.
Film (in het Engels)
Folder
Raadpleeg hier onze folder met raadgevingen na een lumbale discushernia.
Hoe wordt een cervicale discushernia (nekhernia) geopereerd?
De cervicale discushernia of nekhernia is vergelijkbaar met een lumbale hernia: het is een uitpuiling van het zachtere binnengedeelte van de tussenwervelschijf die druk veroorzaakt op de zenuw. Hierdoor straalt de pijn tot in de arm uit. Ter hoogte van de halswervels is ruggenmerg aanwezig, wat een bijkomend risico inhoudt. Als de hernia op het ruggenmerg drukt, is een ingreep sowieso noodzakelijk. Als de hernia alleen op de zenuw drukt, gelden dezelfde regels als bij de lumbale hernia: een ingreep zal worden voorgesteld als de pijn niet verdwijnt na een periode van pijnbehandeling.
De ingreep verloopt anders dan in de lage rug. Bij het grootste gedeelte van de patiënten verloopt de operatie via de voorkant van de wervelzuil (dus via de hals). Meestal wordt de tussenwervelschijf zo goed als volledig verwijderd. Aangezien men de discus (=tussenwervelschijf) volledig wegneemt, wordt deze meestal vervangen door een prothese. Dit zijn de zogenaamde 'cages' (= kooien) uit bio-compatibel materiaal, gevuld met kunstbot of bot uit de botbank.
De wetenschap staat vandaag ver in de ontwikkeling van bio-compatibele materialen. Dit zijn stoffen die in het menselijk lichaam geen reactie veroorzaken.

|
Dit is een cage uit PEEK (gebaseerd op koolstofvezels),
maar ze kan ook uit titanium gemaakt zijn.
|
In sommige gevallen, bvb wanneer verschillende discusniveaus moeten geopereerd worden, kan het nodig zijn om een bijkomende versteviging tussen verschillende wervels aan te brengen. Dit gebeurt door aan de voorzijde van de wervels een metalen plaatje met schroefjes vast te maken. Uw chirurg zal de noodzaak hiervan vooraf met u bespreken.
Het verstijven van een segment heeft echter ook nadelen. Zo kunnen de boven- en onderliggende tussenwervelschijven sneller slijtage vertonen, met soms een nieuwe hernia tot gevolg. Maar dit is zeker niet altijd het geval.
De resultaten van deze ingreep zijn doorgaans uitstekend, de hospitalisatie kort (meestal 1 overnachting na de ingreep).
Film (in het Engels)
Folder
Raadpleeg hier onze folder met raadgevingen na een cervicale discushernia operatie.